Introduction
Acne, a common skin condition affecting millions worldwide, has been known to cause stress and impact self-esteem. It is characterized by the presence of pimples, blackheads, and whiteheads, often resulting from excess oil production, clogged pores, inflammation, and bacterial overgrowth. While numerous treatments are available, exploring unconventional solutions such as probiotics offers hope for those seeking clearer skin.
Probiotics, known for their gut health benefits, are fast emerging as effective potential allies when it comes to acne management. In this article, we will answer some commonly asked questions regarding the connection between probiotics and acne, while offering insights into their effectiveness and practical tips for achieving healthier skin.

What Impact Does the Gut Microbiome Have on Acne? [1]
The impact of the gut microbiome on acne is a fascinating area of research that highlights the interconnectedness of various bodily systems. The gut microbiome refers to the diverse community of microorganisms residing in the gastrointestinal tract, including bacteria, viruses, fungi, and archaea. While traditionally associated with digestion and nutrient absorption, emerging evidence suggests that the gut microbiome plays a significant role in modulating immune function, inflammation, and even skin health.
A balanced gut microbiome helps regulate immune responses to prevent excessive inflammation and autoimmune reactions. Imbalances in the gut microbiome can trigger systemic inflammation which is implicated in the pathogenesis of acne. Chronic inflammation promotes the release of pro-inflammatory cytokines and other mediators that can exacerbate acne symptoms by increasing sebum production, clogging pores, and promoting the proliferation of acne-causing bacteria.
The gut microbiome also plays a role in metabolizing and regulating hormones, including androgens such as testosterone. Androgens are known to influence sebum production and contribute to the development of acne. Imbalances in gut microbiota composition may affect hormone metabolism, potentially exacerbating hormonal acne.
Recent studies have also demonstrated a link between gut health and skin barrier function. A compromised gut barrier, commonly referred to as “leaky gut”, can lead to increased intestinal permeability, allowing harmful substances to enter the bloodstream and trigger systemic inflammation. This systemic inflammation can manifest in the skin and contribute to conditions like acne.
The gut microbiome can also indirectly influence the composition and diversity of the skin microbiome, i.e., the colonies of microorganisms residing on the skin’s surface. Dysbiosis (imbalance) in the gut microbiome may disrupt the balance of the skin microbiome which can potentially trigger the proliferation of pathogenic acne-causing bacteria, i.e., Cutibacterium acnes (C. acnes).

Do Probiotics Help Clear Acne? [2]
Probiotics are microorganisms that support gut health when consumed on a regular basis. Studies exploring their role in acne management reveal promising results. These beneficial bacteria contribute to a balanced gut microbiome, influencing various bodily functions including immune regulation and inflammation control. Probiotics like Lactobacillus and Bifidobacterium strains have shown potential in reducing acne severity by modulating immune responses, inhibiting pathogenic bacteria growth, and regulating sebum production. Understanding how probiotics exert their influence on acne requires exploring their mechanisms of action which include:
- Modulation of the Gut Microbiome: Probiotics contribute to a balanced microbiome by promoting the growth of beneficial bacteria and suppressing harmful pathogens, thereby promoting microbial equilibrium in the gut. A balanced microbiome is critically important for immune function, inflammation regulation, and overall health, which includes skin health.
- Immune Regulation: Probiotics interact with the gut-associated lymphoid tissue (GALT) and mucosal immune cells, thereby influencing immune function and systemic inflammation. By modulating immune response, probiotics help to regulate inflammatory pathways implicated in acne development. This immune-regulatory effect may help to reduce the severity and frequency of acne flare-ups.
- Inflammation Reduction: Inflammation is a key driver of acne, contributing to the formation of pimples, blackheads, and whiteheads. Probiotics have been shown to possess anti-inflammatory properties that help to mitigate inflammation both locally in the gut, and systemically throughout the body. By reducing inflammatory cytokines and other mediators, probiotics can help alleviate inflammation associated with acne.
- Inhibition of Pathogenic Bacteria: Certain probiotic strains produce antimicrobial substances that inhibit the growth of pathogenic bacteria, including those implicated in acne development (C. acnes). For example, the above-mentioned Lactobacillus and Bifidobacterium strains can produce organic acids, bacteriocins, and other compounds that create an unfavorable environment for acne-causing bacteria. By competing with and suppressing the growth of these pathogens, probiotics help maintain a healthier skin microbiome which reduces the likelihood of acne flare-ups.
- Regulation of Sebum: Sebum, the oily substance naturally produced by the body’s sebaceous glands, plays a crucial role in acne formation. Excessive sebum production can lead to clogged pores and acne breakouts. Some probiotic strains have been shown to influence sebum production by regulating the activity of sebocytes, i.e., the cells responsible for sebum synthesis. By modulating sebum production, probiotics can help maintain a balanced skin environment, thereby reducing the risk of acne development.
In short, probiotics contribute to clearer skin by promoting a healthy gut microbiome, modulating immune responses, reducing inflammation, inhibiting pathogenic bacteria from proliferating, and regulating sebum production.
How Long Do Probiotics Take to Clear Skin?
The timeline for probiotics to clear a person’s skin can vary widely depending on several factors such as an individual’s gut microbiome composition, the severity of acne, the specific probiotic strains used, dosage, and overall lifestyle factors. While some individuals may experience noticeable improvements with a few weeks of starting probiotic supplementation, others may require several months before seeing significant changes in their skin. Factors that play a role when it comes to the issue of timeliness include:
- Gut Microbiome Composition: Each person’s gut microbiome is unique and is influenced by factors such as genetics, diet, lifestyle, and previous antibiotic use since antibiotics used to treat bacterial infections tend to wreak havoc on the gut microbiome. Individuals with a more imbalanced gut microbiome may take longer to experience improvements as probiotics initially work to restore microbial balance.
- Severity of Acne: The severity and type of acne also play a role in determining how long it takes for probiotics to help clear the skin. Mild cases of acne may respond more quickly to probiotic intervention compared to moderate to severe acne. In severe cases, when multiple factors contribute to acne development, probiotics may take longer to exert their effects, with additional treatments most likely being necessary.
- Specific Probiotic Strains and Dosage: Different probiotic strains have varying mechanisms of action and efficacy in managing acne. Some studies suggest that certain strains, such as those mentioned previously, may be more effective in improving skin health and reducing acne severity. Additionally, the dosage of probiotics can impact their effectiveness. Higher doses may lead to faster results, but individual tolerance levels should be considered to avoid adverse effects.
- Consistency and Duration of Supplementation: Consistent and long-term supplementation is essential for maximizing the benefits of probiotics for skin health. While some individuals experience initial improvements within a few weeks, sustained use over several months may be necessary to achieve long-lasting results. Abrupt discontinuation of probiotics may result in a regression of improvements, emphasizing the importance of ongoing supplementation.
So, if you’re wondering, “Does cleaning your gut clear acne?”, the answer is that while probiotics represent a solution for acne management, patience and consistency are key. It’s essential to set realistic expectations and understand that individual responses may vary. Moreover, probiotics are meant to supplement, and work in concert with, topical solutions and healthy lifestyle habits for maximum effectiveness to be realized.
Which Probiotic Is Best for Skin? [3]
Selecting the best probiotics for skin health involves considering specific strains that have been researched for their efficacy in managing skin conditions like acne. Several probiotic strains have shown promise in improving skin health and reducing acne severity due to their mechanisms of action. Probiotics regarded as beneficial for skin health include:
- Lactobacillus acidophilus: L. acidophilus is one of the most well-known and extensively studied probiotic strains. It is known for its ability to promote gut health by maintaining a balanced microbiome. Studies have shown the L. acidophilus supplementation can help reduce inflammation and improve skin conditions such as acne. Moreover, a recent study found that L. acidophilus reduced the production of sebum, a waxy/oily substance that is known to clog pores when combined with dead skin cells.
- Lactobacillus rhamnosus: L. rhamnosus is another protiotic strain known for its beneficial effects on skin health. Research suggests that L. rhamnosus supplementation may help improve acne by reducing inflammation and inhibiting the growth of acne-causing bacteria like C. acnes. Additionally, L. rhamnosus has been shown to enhance the skin’s natural defenses and promote barrier function, which can help prevent acne breakouts.
- Bifidobacterium bifidum: B. bifidum is a probiotic stratin commonly found in the gut microbiome and has been studied for its potential in managing skin conditions like acne. B. bifidum supplementation may help improve acne by modulating immune responses, reducing inflammation, and inhibiting the growth of pathogenic bacteria on the skin. Additionally, B. bifidum has been shown to support overall gut health, which can indirectly benefit skin health.
- Lactobacillus casei: L. casei is a probiotc strain with anti-inflammatory properties that may benefit skin health. Studies have shown that L. casei supplementation can help reduce inflammatory markers in the body, which may help alleviate symptoms of inflammatory skin conditions like acne. Moreover, L. casei has been show to support gut health and enhance immune function, which can contribute to overall skin health.
- Lactobacillus plantarum: L. plantarum is a probiotic strain known for its ability to support gut health and modulate immune function. Research suggests that L. plantarum supplementation may help improve acne by reducing inflammation and inhibiting the growth of acne-causing bacteria. Also, L. plantarum has been shown to enhance the skin’s natural defenses and promote skin barrier function which too can help prevent acne breakouts.
- Bifidobacterium lactis: B. lactis has demonstrated anti-inflammatory effects which are useful in combating chronic inflammation, a key player in acne formation. By modulating inflammatory pathways and reducing the production of pro-inflammatory cytokines, B. lactis helps to mitigate inflammation and alleviate acne symptoms. B. lactis also plays a role in immune regulation to help the body maintain a balanced immune response to prevent acne-exacerbating excessive inflammation. B. lactis also supports gut barrier integrity by promoting the production of mucin and reinforcing tight junctions between intestinal epithelial cells to prevent harmful substances from leaking into the bloodstream, a condition referred to as “leaky gut”, and causing an inflammatory (acne-triggering) response.
- Bacillus coagulans: B. coagulans produces antimicrobial substances that inhibit the growth of pathogenic bacteria, including those involved in acne formation (C. acnes). By competing with and suppressing the proliferation of acne-causing bacteria, B. coagulans helps maintain a healthier skin microbiome, thereby reducing the likelihood of acne breakouts. B. coagulans also contributes to digestive health by promoting the breakdown of absorption of nutrients to support a balanced gut microbiome.
So, when trying to figure out the best probiotic for acne, it’s important to choose products that contain specific strains, or combinations of strains, that have been vetted for their effects on acne and skin health. Additionally, factors like dosage, product quality, and individual tolerance should be considered as well. Consulting with a healthcare professional can help determine the most suitable probiotic regimen based on individual needs and preferences.
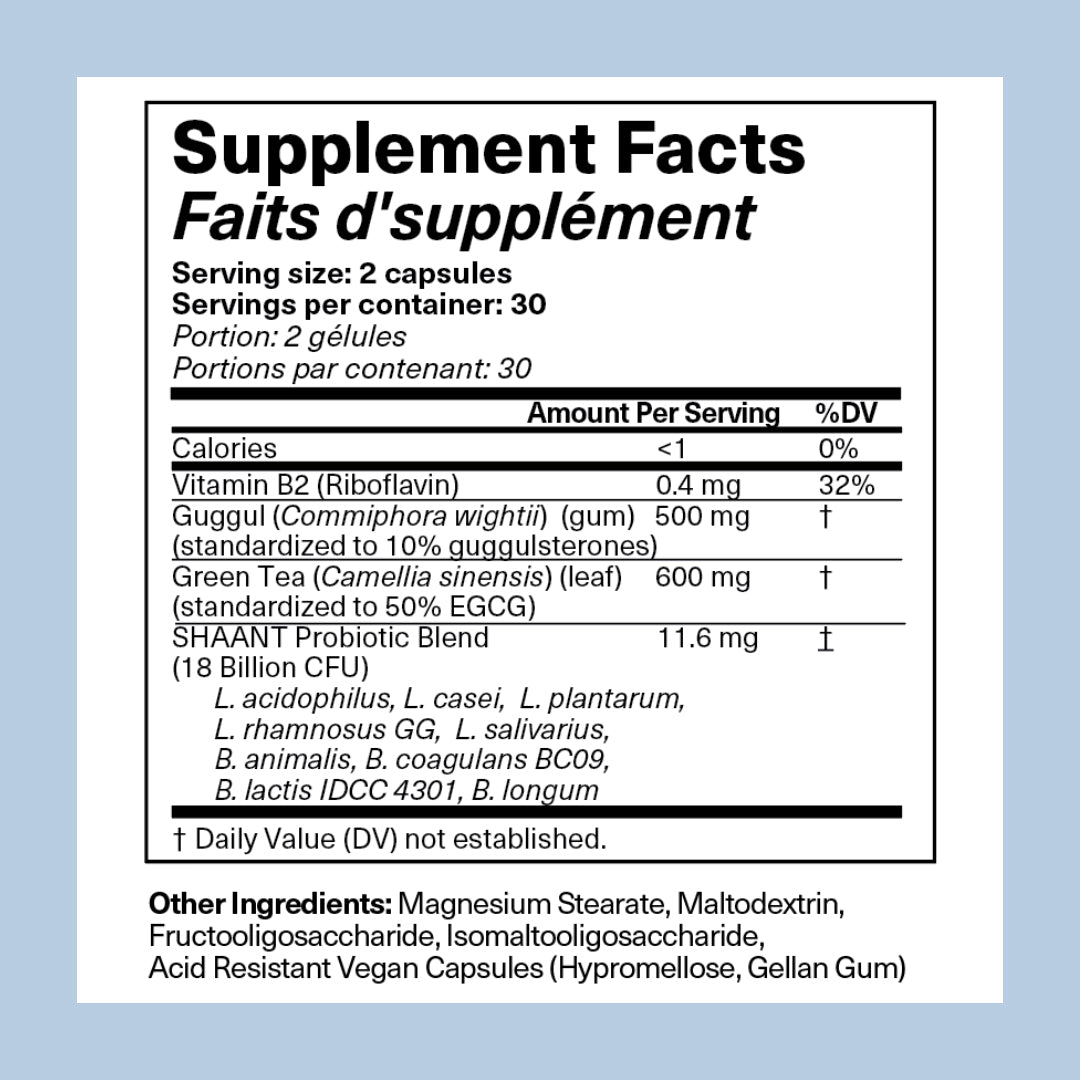
It should also be noted that research, including our own, has shown that combining probiotics with antioxidant plant medicinals yields even greater benefits. One such example is Guggul, an herb that has been shown to help reduce blood lipid levels and lower blood sugar levels. Guggulsterones, one of the active ingredients found in Guggul, have been found to decrease acne lesions in a manner comparable to the commonly used antibiotic tetracycline! [4]
Another example is epigallocatechin gallate (EGCG), a potent antioxidant derived from green tea extract, has both anti-inflammatory and antioxidant properties. In various studies, subjects suffering from acne were found to have experienced a significant reduction in acne lesion counts. This surprising result was achieved by merely consuming ECGC on a consistent basis. [5]
What Is the Skin-Gut-Brain Axis? [6]
The famous Greek physician Hippocrates (think Hippocratic oath) believed that “All disease begins in the gut.” As it turns out, his belief appears to be spot on! Recent studies have confirmed the existence of a strong physiological/biological relationship between skin health, gut health, and emotional health. The bidirectional connections between these three organ systems are referred to as the “skin-gut-brain axis”.
It has been found that most individuals suffering with skin conditions like acne, eczema, and rosacea, i.e., inflammatory skin disorders, also experience gastrointestinal issues. An unbalanced (in terms of quantity and/or diversity of microorganisms) gut microbiome has been found to promote the release of a compound known as “substance P”, a neuropeptide produced in a person’s brain, gut, and skin. Substance P is known to increase inflammation-triggering histamine levels in the skin which leads to an over-production of pore-clogging sebum, a precursor to acne flare-ups.
Probiotics have been shown to suppress the production of substance P, thereby cutting off a primary cause of inflammatory skin conditions like acne, i.e., inflammation! Further support for the existence of a connection between the skin and gut is based on a showing that oral probiotics can decrease the production of lipopolysaccharide, an endotoxin produced in the gut, that can trigger acne and other skin problems by way of, you guessed it, inflammation! Hence, science appears to have affirmatively established a connection between the skin and the gut, i.e., the skin-gut axis.
Recent studies have also established the existence of a skin-brain connection (skin-brain axis) by validating the impact that psychological stress has on an individual's skin. Here too, conditions such as acne, psoriasis, and atopic dermatitis (eczema) are oftentimes triggered and/or exacerbated by chronic psychological stress caused by the brain’s release of stress hormones (ex. Cortisol) and other inflammatory factors, (ex. substance P), which can lead to stress-induced inflammatory skin conditions.
Regarding the bidirectional communication engaged in by these organs because skin is continuously exposed to the environment, it’s naturally more susceptible to environmental stressors which can trigger the release of stress hormones. For example, when skin is exposed to UV light and/or extreme outside temperatures, it produces stress hormones that send a signal to the brain which leads to, you guessed it again, inflammation. In short, psychological stress (via the brain) can contribute to inflammatory skin disorders, while environmental stressors (via the skin) can contribute to psychological stress.
The last piece of the puzzle involves the relationship between the gut and the brain (gut-brain axis), the existence of which is pretty much a no-brainer (pun intended). As we already know all too well, an upset stomach has an immediate effect on a person’s mental wellbeing based on the signals sent by the gut to the brain. Similarly, mentally stressful situations tend to cause an upset stomach based on the signals sent by the brain to the gut. We’ve all, unfortunately, experienced these phenomena on more occasions than we care to remember.
Hence, the existence of a skin-gut-brain axis whereby all three organ systems communicate with, and physiologically influence, one another is well established. When one of these systems experiences a problem, like the gut, it triggers a kind of biological inflammatory domino effect which oftentimes leads to an acne flare-up and/or makes an existing acne breakout worse.
Conclusion
For those still wondering How Do I Get a Healthy Gut for Clear Skin? the answer is to make sure that you have the right amount, and types, of microorganisms in your gut microbiome. While this is typically accomplished by eating a variety of probiotic-rich, plant-based foods like fruits, vegetables, nuts, seeds, and legumes (beans), most individuals fail to follow and/or consistently adhere to such a dietary regimen. This is where probiotic supplementation comes into play.
The role of probiotics for skin acne management offers a promising avenue for achieving clearer skin. Understanding their influence on gut health and the gut-skin axis underscores their relevance in addressing acne’s underlying factors. While probiotics may not offer “immediate” results, consistent supplementation, coupled with dietary and lifestyle modifications, can yield long-term skin benefits. It should also be noted that studies are currently ongoing to validate the usefulness of probiotics on acne, and skin health in general, through the application of probiotics directly on the skin surface to help balance the skin microbiome (more on that later).
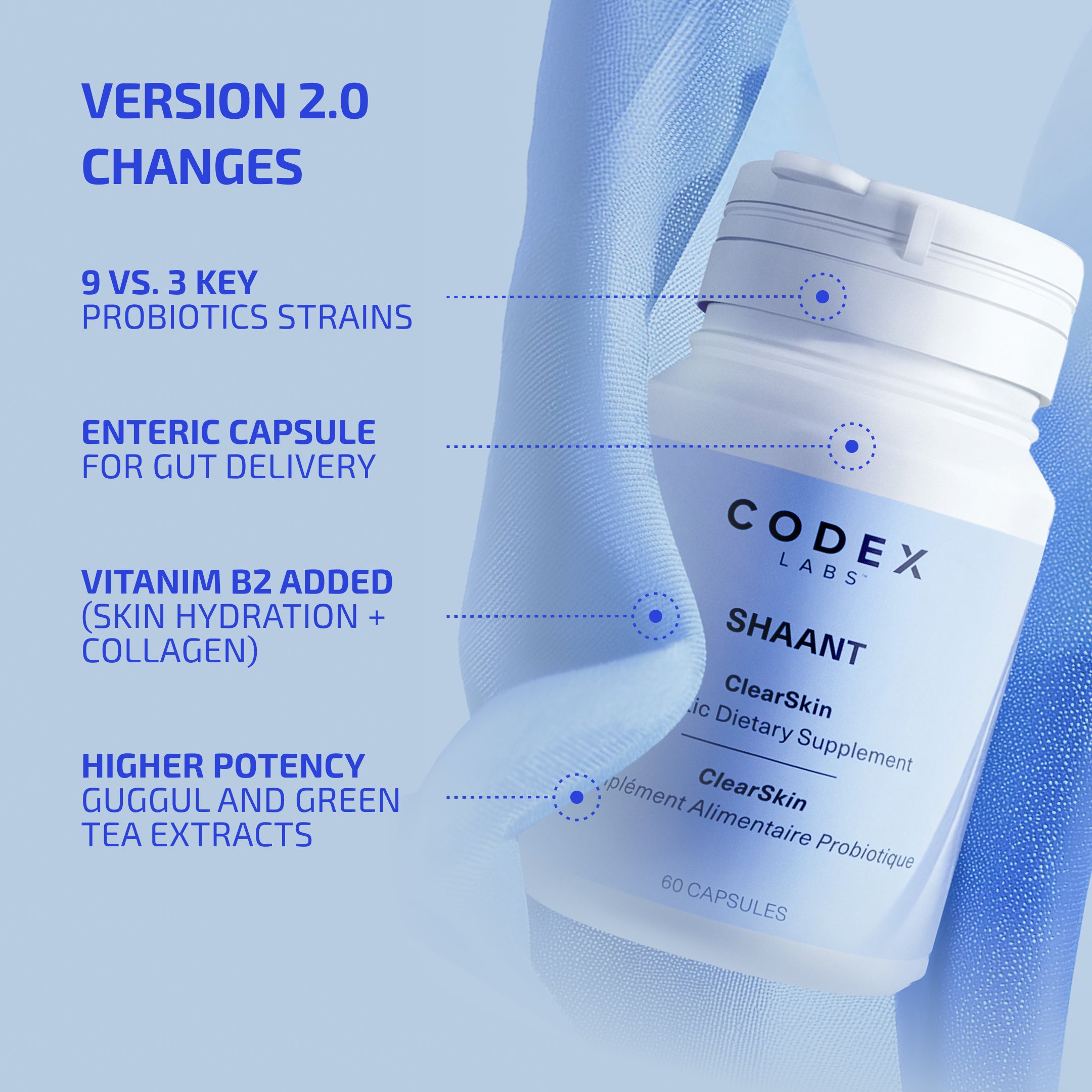
Here at Codex Labs, the copious amounts of research conducted by our product development team helped us to realize that an “integrative” approach to skincare health that addresses the inside of a person’s body, as well as the skin’s surface, represents the most holistic and efficacious strategy for achieving skin that looks as good as it feels. The results of our R&D efforts are embodied in our patent-pending dietary supplements SHAANT® SKIN DE-STRESS for hormonal acne, and SHAANT® CLEAR SKIN PROBIOTIC for bacterial acne. These dietary supplements not only contain the types of probiotic for acne strains that have been scientifically vetted for their ability to help manage acne-prone skin, but also contain potent plant-based antioxidants which have been shown to address a primary cause of acne, INFLAMMATION!
The combination of these oral probiotic supplements, together with our SHAANT® COLLECTION line of topical skincare products, represents the one-two, inside-out skincare strategy your acne prone skin has been craving. And, to help you monitor the progress of your chosen acne treatment products and strategies, you may want to take advantage of Codex’s precision skin health platform SGBNET® and its acne lesion tracking tool, DERMSCORE™, an AI-powered, mobile phone operated skin analyzer that will help you keep track of the progress being made on your pimples/pustules. And because it’s FREE to use you literally have nothing to lose, other than future acne flare-ups.
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6678709/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8953587/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10385652/#:~:text=Different%20probiotics%20can%20treat%20different,Streptococcus%20thermophilus%20and%20Lactobacillus%20johnsonii
- https://pubmed.ncbi.nlm.nih.gov/7798429/
- https://pubmed.ncbi.nlm.nih.gov/23096708/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9979212/#:~:text=In%20the%20last%20decade%2C%20the,%2Dpsychological%20disorders%20(2).