Introduction
When most people think about the side-effects of cancer treatment, hair loss often comes to mind first. Yet for many patients, disruptions to skin health can be just as distressing and oftentimes quite uncomfortable. Conditions such as radiation- or chemo-induced dermatitis are two of the most common cancer treatment skin side effects, producing symptoms that range from mild redness and dryness to severe discomfort involving peeling, blistering, and open sores.
Both radiation therapy and chemotherapy affect rapidly dividing cells, including those responsible for maintaining a healthy skin barrier. As a result, many individuals experience chemotherapy skin irritation or localized radiation injuries causing itching, burning, inflammation, and compromised skin barrier integrity. These changes can negatively impact confidence, sleep quality, and overall wellbeing throughout the cancer treatment process.
In this article, we’ll explore the real-world impact of skin dermatitis during cancer treatment, examining why it develops, how to identify early warning signs, available treatment options which include evidence-based radiation dermatitis treatment strategies, and last but not least, ways in which patients can support their skin barrier safely and effectively.

What Is Skin Dermatitis During Cancer Treatment? [1]
Skin dermatitis during cancer therapy relates to inflammation, irritation, and a breakdown of the skin barrier that occurs as a direct result of medical oncologic treatments. Unlike traditional eczema or allergic contact dermatitis, this condition which is oftentimes categorized as chemo-induced dermatitis or radiation-induced dermatitis, stems from the cellular damage triggered by chemotherapy, radiation therapy, targeted therapy, or immunotherapy.
These “forms” of dermatitis appear when the treatment causes disruptions in:
- Healthy skin cell regeneration
- Sebaceous oil production
- Natural hydration mechanisms
- Immune signaling within the skin barrier
- Microbiome
Radiation-Induced Dermatitis
Radiation dermatitis, commonly called radiation-induced dermatitis, develops when ionizing radiation damages the skin barrier in the precise area exposed to the therapy. Since radiation targets fast-dividing cells, the epidermal regeneration cycle slows dramatically. When cellular regeneration/replacement cannot keep pace with the injury caused by the treatment, visible skin breakdown occurs.
Typical symptoms include, for example:
- Redness and inflammation
- Dry, flaky skin
- Tightness or burning sensations
- Peeling or weeping skin
- Manifestation of blisters or ulcers in severe cases
Notably, radiation dermatitis occurs only in the treatment field, meaning the rash forms in the same shape and location as radiation exposure.
Chemo-Induced Dermatitis
Chemo-induced dermatitis, on the other hand, is triggered by the systemic effects of anti-cancer medications circulating within the bloodstream. Instead of remaining localized (like radiation), this form of rash may appear on various areas of the body, making chemotherapy skin irritation a particularly widespread concern.
Symptoms can include:
- Diffuse red or inflamed rashes
- Acne-like eruptions on the face and torso
- Intense itching or tenderness
- Peeling skin on hands and feet
Unlike radiation-induced dermatitis, which develops slowly, chemotherapy skin irritation may emerge suddenly during, or shortly after, a treatment cycle.
Who Is Most at Risk?
Certain populations have a heightened likelihood of developing severe cancer treatment side effects, including:
- Individuals with fair or sensitive skin
- Patients receiving combination therapies
- Those with pre-existing inflammatory skin disorders (eczema, psoriasis, rosacea, etc)
- Immuno-compromised individuals
- Patients exposed to sun, heat, friction, or irritants during therapy
Causes of Treatment-Related Dermatitis
Multiple biological mechanisms contribute to the development of dermatologic side-effects of cancer treatment:
1. Radiation Injury
With radiation-induced dermatitis, oxidative stress damages skin DNA and proteins. This process compromises sweat glands, sebaceous glands, collagen production and the skin barrier in general leaving skin thin, dry, and less resilient to friction.
2. Chemotherapy Toxicity
Chemo-induced dermatitis develops as various chemotherapeutic agents impair skin regeneration and alter inflammatory signaling. These effects can lead to:
- Ongoing redness
- Cracking or scaling skin
- Nail separation or pigmentation loss
- Sensory irritation, burning, or itching
3. Immunotherapy Reactions
Some therapies overstimulate immune responses, producing rashes similar to autoimmune dermatitis. These immune-mediated eruptions represent the more intense cancer treatment skin side effects which may require prescription medications for relief.
4. Environmental Triggers
Radiation and chemotherapy leave skin extraordinarily sensitive to additional stressors including, for example:
- Sun exposure and heat
- Tight clothing or friction
- Fragrance-containing soaps
- Alcohol-based products
- Poor nutrition or hydration
- Emotional stress
Symptoms and Identification [2]
Common Symptoms
Patients experiencing radiation-induced dermatitis or chemo-induced dermatitis often report:
- Redness or darkening pigmentation
- Dry patches or scaling
- Intense itching or burning sensations
- Peeling or shedding skin
- Skin tightness or pain
- Blistering or ulceration in severe cases
How to Differentiate Common Reactions
|
Feature |
Radiation-Induced |
Chemo-Induced |
Allergic Rash |
|
Distribution |
Radiation site |
Widespread |
Diffuse |
|
Onset Timing |
Gradual |
Sudden |
Rapid |
|
Pain |
Common |
Variable |
Rare |
|
Appearance |
Peeling, shiny, raw |
Acneiform/scaly rash |
Raised hives |
Areas Frequently Impacted
- Chest and breasts
- Neck and jaw line
- Pelvic and abdominal region
- Face and scalp
- Palms and soles
Treatment Options [3]
Clinical Treatments
Effective management focuses on reducing inflammation and protecting the skin barrier. Evidence-based approaches to both chemo-induced dermatitis and radiation-induced dermatitis treatment options include:
Topical Therapies
- Low-potency corticosteroids
- Ceramide-rich repair creams
- Petrolatum-based barrier ointments
- Protective wound dressings or hydrogel pads
Oral Treatments
- Antihistamines for itching
- Antibiotics for secondary skin infections
- Immunosuppressants for immune-mediated rashes
Radiation-Specific Care
Best practices for radiation-induced dermatitis treatment include:
- Regular “gentle” cleansing
- Use of non-adherent (sticky) dressings
- Controlled application of medicated creams
- “Strict” sun protection
Lifestyle and Home Management
- Bathe in lukewarm water “only”
- Avoid scrubbing the skin
- Moisturize 2–3 times daily
- Wear loose cotton clothing
- Maintain hydration
- Avoid sun exposure on affected areas
When to Seek Medical Attention
Consult your care team if skin reactions cause:
- Persistent pain
- Open wounds
- Signs of infection
- Spreading inflammation
- Sleep disruption
Prevention Strategies [4]
While not all skin reactions can be prevented, early intervention greatly reduces severity.
Proactive Skin Care
- Begin skin barrier repair/maintenance routines before therapy starts
- Choose fragrance-free, highly gentle cleansers
- Use mineral sunscreen daily
- Avoid the use of retinoids or chemical exfoliants
Lifestyle Support
- Adequate hydration
- Protein-rich, nutrient-dense diets
- Routine sleep schedules
- Gentle movement and stress reduction
Myths and Facts
Myth: Chemo rashes mean treatment is dangerous.
Fact: Chemo-induced dermatitis is common and manageable with medical supervision.
Myth: Sun exposure helps radiation burns heal.
Fact: UV exposure “worsens” injury and delays healing during radiation dermatitis treatment.
Myth: Avoid creams during therapy.
Fact: Emollients are essential for preventing worsening cancer treatment side effects.
Oncology-Focused Support Kit
Skincare Barrier Support Kit
Oncology-focused skincare products are designed to protect compromised skin barriers during both chemo-induced dermatitis and radiation-induced dermatitis flare-ups. A typical support kit includes:
- Ultra-gentle cleanser
- Ceramide barrier moisturizer
- Occlusive healing ointment
- Broad-spectrum mineral sunscreen
Section 9: Frequently Asked Questions
1. What causes chemo-induced dermatitis?
Systemic chemotherapy toxicity which triggers inflammatory skin responses.
2. How long does radiation-induced dermatitis last?
Typically, several weeks after radiation ends.
3. Is chemotherapy skin irritation permanent?
No, most rashes resolve after treatment is completed.
4. What helps radiation dermatitis treatment at home?
Skin barrier repair/maintenance products, gentle cleansing, cooling pads, and sun protection.
5. Should blisters from cancer treatment be popped?
No, absolutely not, as this increases infection risk.
6. Can skin reactions pause treatment?
Severe cases occasionally require dose delays.
7. Can sunscreen be used during radiation therapy?
Yes, with mineral-based sunscreens being most recommended.
8. Does rash mean treatment isn’t working?
No, skin reactions reflect tissue sensitivity, not treatment success.
9. Can chemo rash spread to the scalp?
Yes, especially when it comes to targeted therapies.
10. Should dermatologists be part of oncology care?
Yes, since early dermatology involvement tends to improve outcomes.
Conclusion
Skin reactions represent one of the most common, and treatable, side-effects of cancer treatment. Both chemo-induced dermatitis and radiation-induced dermatitis reflect “temporary” skin barrier injury, rather than treatment failure. With early recognition, proactive skin care treatment, and overall skin barrier support, various cancer treatment side effects can be managed effectively.
Proactive dermatologic care reduces the discomfort of chemotherapy skin irritation, protects the skin’s integrity, and improves patient quality of life during a very demanding chapter of healing.
Call to Action
For those navigating the unpleasant journey of cancer treatment involving chemo- and/or radiation therapies, Codex Labs has developed technologies that bring much needed relief to therapy-compromised skin. These include:
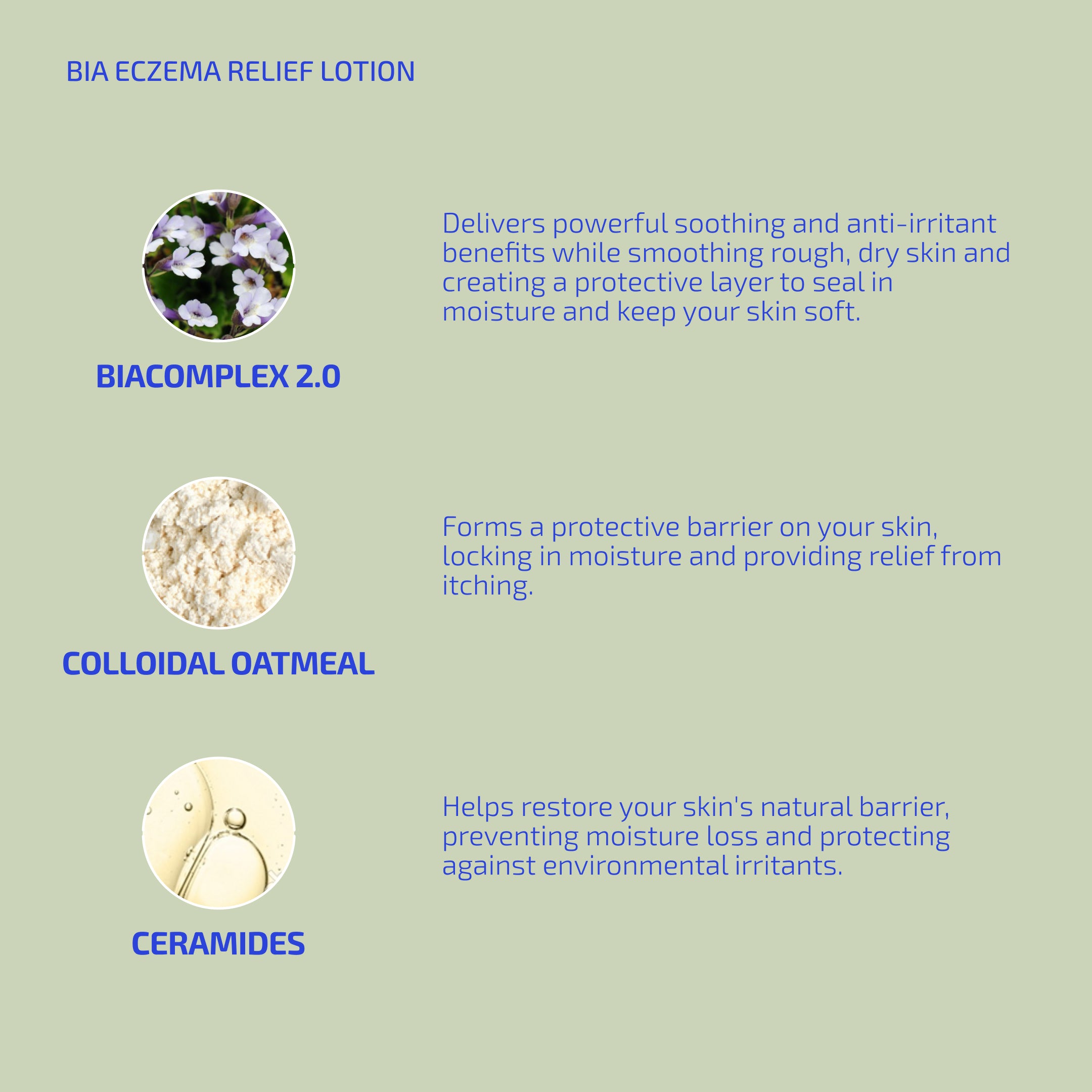
· BIA ECZEMA RELIEF LOTION – A soothing lotion containing our patented BiaComplex 2.0 that deeply hydrates and protects itchy, flaky, dry, sensitive therapy-compromised skin.
· BIA CLEANSING OIL (for face) – A soothing cleansing oil that cleanses without stripping moisture or changing skin pH in the most sensitive skin.
· SHAANT FOAMING CLEANSER (for makeup removal) – An oil-free, foaming, micellar water-based cleanser that soothes, refines the appearance of pores, and reduces oiliness without stripping moisture or the skin’s microbiome.
· BIA UNSCENTED SOAP – A fragrance-free, pH-balanced, microbiome-supporting soap that gently cleanses, softens, and protects skin without irritation.
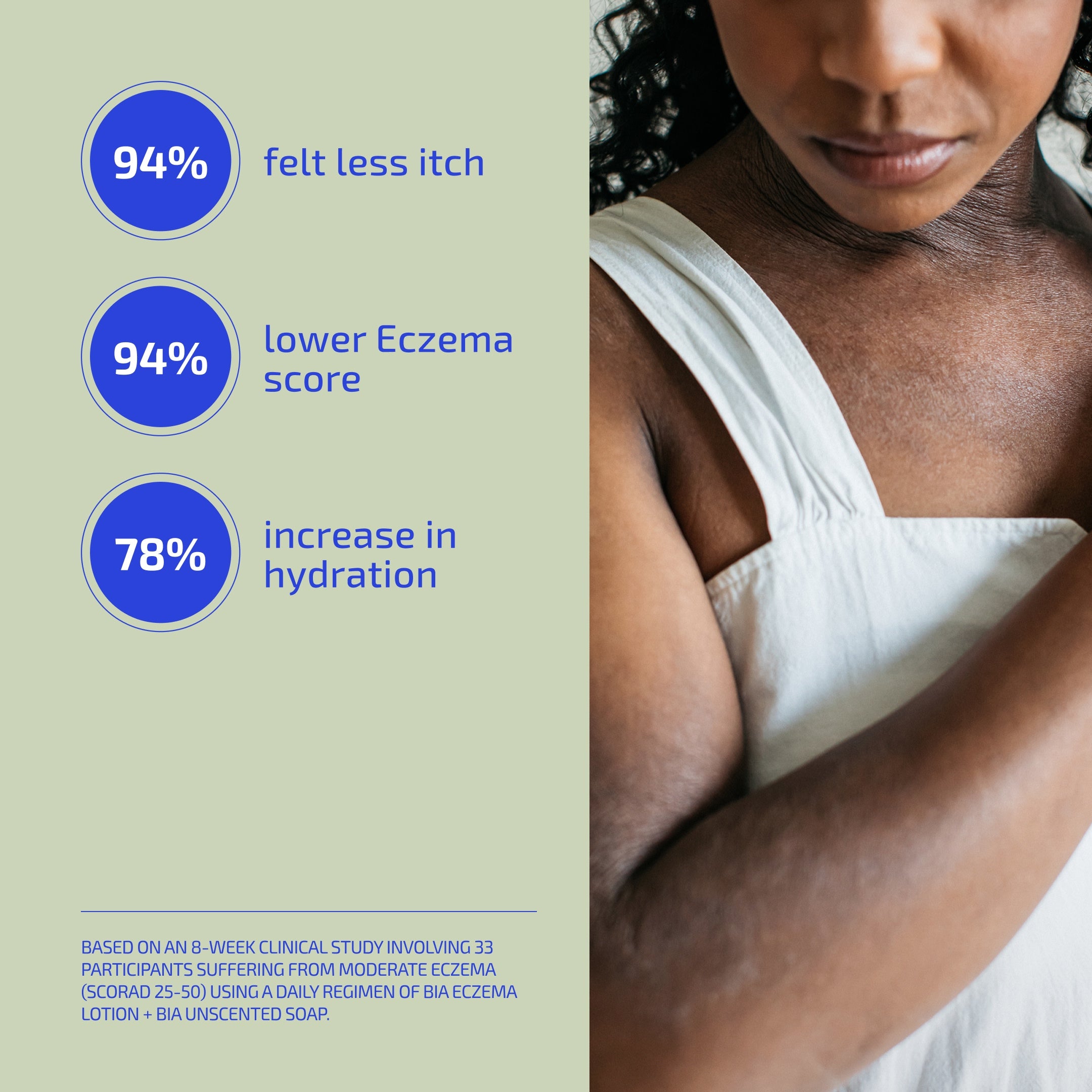
These products will help bring much needed relief to skin suffering the side effects of cancer therapy treatments. How can we be so sure? Because we have the clinical data to prove it!
References:
1. https://www.cancer.org/cancer/managing-cancer/side-effects/hair-skin-nails/rashes-skin-changes.html
2. https://www.cancer.gov/about-cancer/treatment/side-effects/skin-nail-changes