Introduction
When it comes to acne-prone skin, most of us instinctively think and look outwardly at the surface of our skin, focusing on the influence of skincare routines, makeup habits, and environmental stressors on our condition. But what if the key to clearer skin lies deeper within, more particularly, in your gut? Emerging science reveals that the health of your gut microbiome may significantly impact your skin's condition, especially when it comes to acne. This gut-skin connection is not just a trendy topic in holistic health circles—it’s backed by growing clinical evidence.
In this blog article, we’ll explore how gut health influences acne-prone skin, explain the science in simple terms, and offer actionable solutions to help mitigate the condition. We’ll also highlight supplements for hormonal acne and how ingredients can help to maintain clear skin during hormonal shifts. So, let’s dive into this fascinating intersection of dermatology and digestive health.

What is Acne and How Is It Related to Gut Health? [1]
Acne vulgaris is a chronic inflammatory skin condition that primarily makes its presence known on a person’s face, chest, and back. It is characterized by blackheads, whiteheads, papules, pustules, cysts, and nodules. While acne is most common amongst teenagers it can, and unfortunately oftentimes does, persist into adulthood as it is influenced by various internal (inside the body) and external (environmental) factors.
The gut-skin axis is a bidirectional communication network between your gastrointestinal system and your skin. Think of it as a kind of phone line, i.e., your gut sends biological messages to your skin via your immune system, hormones, and metabolites. When your gut microbiome, home to trillions of bacteria, becomes imbalanced, a condition known as “dysbiosis”, it can trigger systemic inflammation via its biological communication pathways which, in turn, oftentimes trigger an acne breakout.
Teens and young adults are the most commonly affected demographic when it comes to acne. That said, hormonal acne triggered by a hormonal imbalance within the body oftentimes associated with menstruation, is particularly prevalent in women between the ages of 20 and 40, and it’s this particular demographic that may benefit the most from addressing gut health as part of a holistic or integrative treatment plan for addressing acne-prone skin.
Causes of Acne and the Role of Gut Health [2]
Primary Causes of Acne
Hormonal fluctuations: Increased androgen levels have been shown to stimulate sebum (oil) production.
- Genetics: A person’s family history plays a significant role in the drama known as acne-prone skin.
- Diet: High glycemic foods, i.e., those that cause a sudden spike in blood sugar levels (ex. starchy and sugary foods), as well as dairy, may worsen existing acne or trigger a new breakout.
- Stress: Alters hormone levels within the body via the release of cortisol and adrenaline which, in turn, activates inflammatory responses which can trigger or worsen acne.
- Microbiome imbalance: Dysbiosis in the gut (imbalance between the number of good versus bad organisms) can also promote acne triggering skin inflammation.
How the Gut Contributes to Acne
- Increased Intestinal Permeability ("Leaky Gut")
When the gut lining becomes compromised, i.e., the junctions between cells that line the gut wall become loose rather than remaining tight, harmful bacteria and toxins can leak through the gut wall and into the bloodstream, thereby triggering immune responses that cause and contribute to systemic inflammation, including in the skin.
- Microbiome Dysbiosis
A healthy gut contains a balanced mix of "good" and "bad" bacteria. When this balance is disrupted (due to antibiotics, poor diet, or stress), it can affect nutrient absorption, immune function, and hormone regulation, all of which are directly tied to skin health.
- Nutrient Malabsorption
An unhealthy gut struggles to absorb essential vitamins and minerals like zinc, vitamin A, and omega-3 fatty acids. These nutrients are known to play a role in helping to prevent acne breakouts.
- Hormonal Imbalances
Specific types of gut bacteria help to metabolize hormones like estrogen. If the gut isn’t functioning optimally, excess hormones may circulate longer within the body, thereby potentially further exacerbating hormonal acne.
Symptoms and Identification
Common Acne Symptoms:
- Red, inflamed pimples
- Clogged pores (blackheads and whiteheads)
- Deep, painful cysts or nodules
- Post-inflammatory hyperpigmentation or scarring
Acne vs. Other Skin Conditions:
Unlike rosacea or perioral dermatitis (a red, bumpy rash around one’s mouth), acne is characterized by pores clogged with sebum (oil) which oftentimes gets worse when associated with hormonal shifts within the body such as those caused by menstruation.
Where It Appears:
- Hormonal acne typically presents along a person’s jawline, chin, and neck.
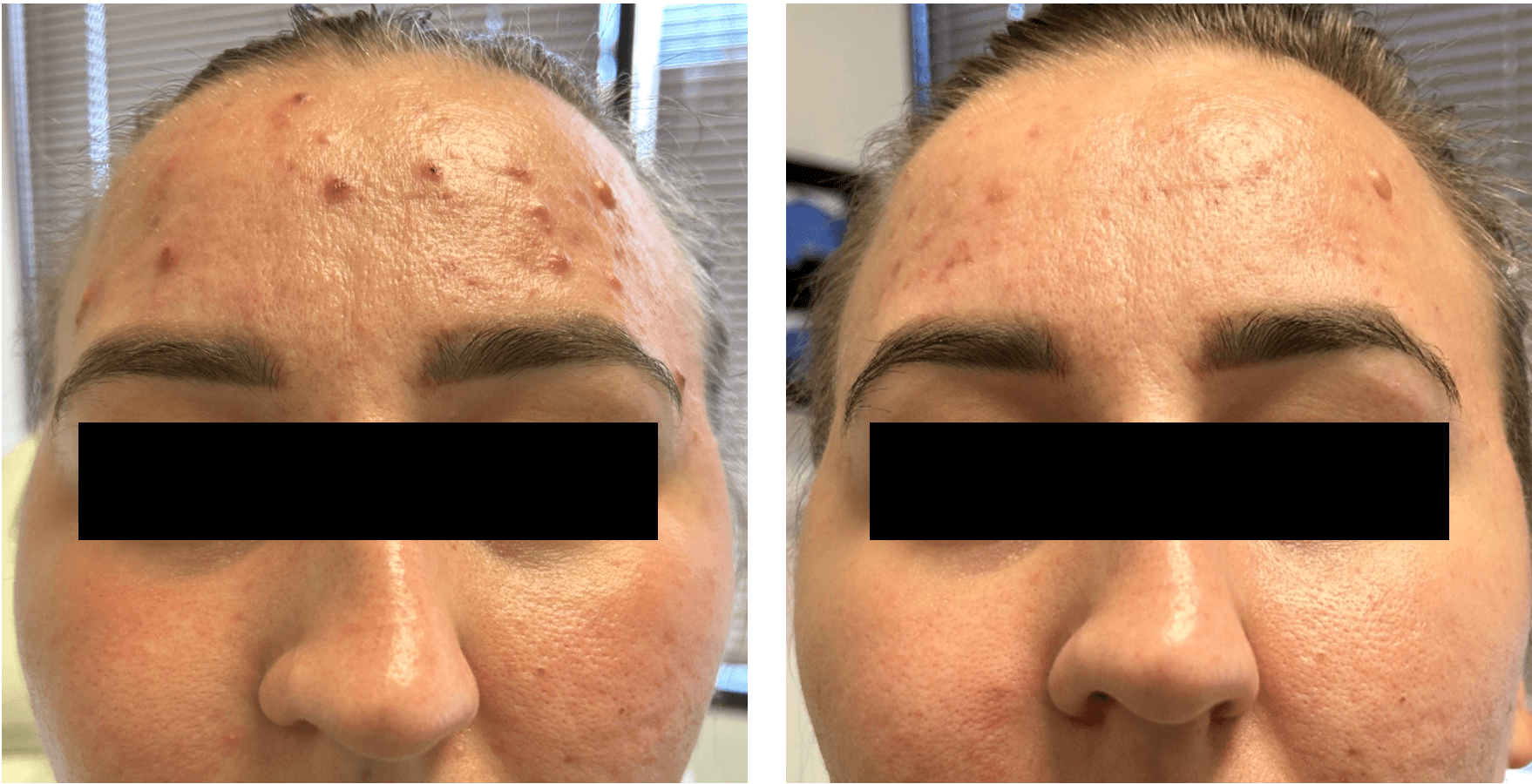
- Gut-related acne is more widespread and may appear on a person’s cheeks, forehead, chin, and upper back area.
Treatment Options
Topical treatment active ingredients conventionally include:
- Benzoyl peroxide: While considered for many years to be the gold standard for treating acne, it has recently come under intense scrutiny due to its alleged potential for releasing cancer causing benzene, coupled with the damage it does to a person’s skin microbiome by killing acne causing bacteria (C. acnes) together with any GOOD bacteria it also contacts
- Salicylic acid: Acts as an exfoliant to remove dead skin cells and unclog pores
- Sulfur: Mother Nature’s powerful acne treatment hero ingredient
- Retinoids: These active ingredients help to reduce oiliness, unclog pores, and promote skin cell turnover (the body’s natural exfoliation process).
Oral Medications:
- Antibiotics: Only intended for short-term use so as to avoid potential treatment resistance issues in the future
- Hormonal treatments: Products like birth control pills or spironolactone can help to mitigate acne breakouts
- Isotretinoin (Accutane): A type of retinoid medication that should only be used as a last resort for severe cases when other, less aggressive treatment options, have failed
The Gut-Health Focused Approach: [3]
- Probiotics: Help to reinforce the gut barrier, thereby helping to reduce systemic inflammation.
- Prebiotics: Nature’s food source for feeding the good “beneficial” bacteria in the gut microbiome.
- Synbiotics: Supplements that contain a combination of pre- and probiotics for the best of both worlds when it comes to gut microbiome management and support.
- Digestive enzymes: These help to enhance nutrient absorption within the gut which can have a positive effect on acne-prone skin.
Lifestyle Changes:
- Adopt a low-inflammatory diet that is rich in fiber, healthy fats, and has a low-glycemic index.
- Reduce your daily intake of dairy and sugar.
- Practice stress reduction techniques such as yoga, meditation, and mindfulness.
- Get adequate sleep on a consistent basis.
When to See a Dermatologist:
- If over-the-counter treatments don’t help after 2–3 months.
- If acne is severe, painful, or causes scarring.
- To discuss personalized, gut-focused treatment plans.
Prevention Strategies
Gut-Friendly Skincare Tips:
- Avoid the use of harsh cleansers that can strip the skin barrier of its natural, moisture retaining oils.
- Use gentle, pH-balanced products on your skin in order to support your skin’s microbiome.
- Make sure to moisturize consistently in order to maintain and support your skin barrier.
Diet and Lifestyle:
- Eat fermented foods rich in probiotics such as yogurt, kimchi, and kefir to help support and manage your gut microbiome.
- Avoid highly processed foods (you know the types this refers to).
- Take probiotic supplements that contain good/beneficial strains of bacteria like Lactobacillus rhamnosus and Bifidobacterium lactis.
- Incorporate histidine, an essential amino acid that the body uses to support gut health and skin repair.
Daily Routine:
- Stick to a consistent sleep schedule.
- Manage stress levels.
- Hydrate properly and consistently.
Myths and Facts
Myth 1: Probiotics are just for digestion
Fact: Probiotics influence the body’s immune function and can therefore help with acne-prone skin
Myth 2: Only teenagers get acne
Fact: Hormonal acne in adults is very common, especially in women (ex. hormonal acne)
Myth 3: All supplements work the same
Fact: Clinical-grade supplements like those with histidine have specific skin benefits
Myth 4: Harsh scrubs fix acne
Fact: Over-exfoliating can damage the skin barrier, cause inflammation, and potentially trigger a breakout
FAQ
1. Can gut health affect acne?
Yes. Gut imbalances can cause inflammation and hormonal disruptions that can trigger acne breakouts.
2. What supplements help with hormonal acne?
Supplements that contain probiotics, zinc, omega-3s, and amino acids like histidine can help regulate gut health and reduce breakouts.
3. What is the gut-skin axis?
It’s the two-way communication between the gut and skin involving hormones, immune signals, and microbiome.
4. How do I know if my acne is hormonal?
Look for cyclical breakouts around the chin and jaw which oftentimes get worse around menstruation.
5. Is histidine good for acne?
Yes. Histidine supports the integrity of the gut lining thereby helping to mitigate inflammation in the skin.
6. Are probiotics useful for those with acne-prone skin?
Yes, especially strains like L. rhamnosus and B. bifidum, which have been found to potentially help regulate inflammation and the body’s immune system.
7. Can diet alone clear acne?
Not always, but a gut-friendly, anti-inflammatory diet can greatly improve skin health and appearance over time.
8. What foods are best for gut health and acne?
Fiber-rich fruits and vegetables, fermented foods, omega-3-rich fish, and plenty of water.
9. Can stress impact gut health and acne?
Absolutely. Stress alters your gut flora and increases inflammation, which can exacerbate breakouts.
10. How long does it take to see improvements with gut health changes?
You may see small improvements in 2–4 weeks, but it often takes 8–12 weeks for significant changes.
Recommended Product or Kit
For those suffering from hormonal acne, Codex Labs’ SHAANT® HORMONAL ACNE SET may be just what the doctor ordered! This dermatologist-developed system is specifically formulated to effectively address hormonal and gut-related acne-prone skin. It’s a science-backed, inside-out approach designed for people who want to address the root causes of hormonal acne, as well as the symptoms.
In addition, and because of the significant impact a person’s skin barrier function has on acne-prone skin, there is the ANTU® SKIN BARRIER SUPPORT SUPPLEMENT with its potent M3™ antioxidant blend coupled with the gut lining + skin barrier supporting amino acid L-histidine, which helps to keep your skin barrier in tip-top shape and your acne-prone skin looking and feeling its best.
Conclusion
It turns out that a person’s gut and skin are more connected than we ever imagined. By nurturing your gut microbiome with diet, supplements, and lifestyle changes, you may see a transformative improvement in your skin health, especially if you happen to suffer from acne-prone skin. If you have NOT yet gifted your acne-prone skin with Codex Labs’ inside- out approach to skin that looks as great as it feels, NOW IS THE TIME!
References
1. https://pmc.ncbi.nlm.nih.gov/articles/PMC6678709/
2 https://cdhf.ca/en/acne-and-digestive-health/
3. https://www.nutritionist-resource.org.uk/articles/gut-health-and-acne-what-you-need-to-know